Scientists at City of Hope have made a groundbreaking discovery by developing universal donor stem cells that could potentially revolutionize therapy for children with lethal brain conditions like Canavan disease, as well as individuals suffering from degenerative diseases such as Alzheimer’s and multiple sclerosis. The findings of this research study were recently published in Advanced Science.
According to Yanhong Shi, Ph.D., chair of the Department of Neurodegenerative Diseases and the Herbert Horvitz Professor in Neuroscience at Beckman Research Institute of City of Hope, this innovative “off-the-shelf” approach has the potential to significantly improve the quality of life for cancer patients who experience cognitive impairment or impaired motor function as side effects of chemotherapy or radiation. Dr. Shi, who has dedicated 12 years to this research, believes that this technique can offer lifesaving treatments to patients in need three to six months earlier.
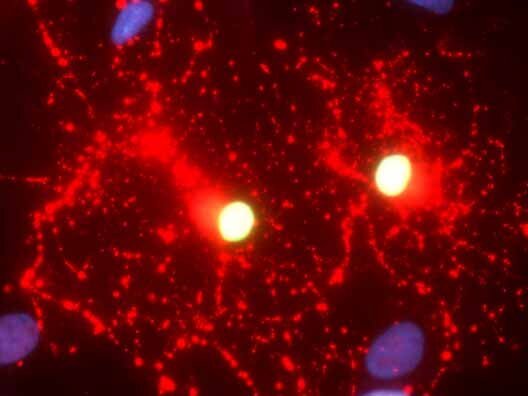
This groundbreaking achievement marks the first time that stem cells have been engineered to function as universal donors for cell therapy, specifically targeting diseases of the central nervous system. The researchers at City of Hope successfully transformed healthy human skin cells, containing the functional aspartoacylase (ASPA) gene, into induced pluripotent stem cells (iPSCs). These iPSCs were then differentiated into oligodendroglial progenitor cells, which are the precursor cells responsible for producing myelin—a protective sheath that surrounds nerve fibers and facilitates the rapid transmission of information along neuronal axons.
In animal models of Canavan disease, the treated mice exhibited significantly increased ASPA activity compared to the control mice. Additionally, they showed a reduction in the toxic accumulation of the metabolite N-acetyl-L-aspartate (NAA) in the brain. Excessive levels of NAA have been linked to impaired motor function, mental deficiencies, and premature death. As a result of the treatment, the mice demonstrated improved myelination and substantially enhanced motor function. Importantly, the universal donor cells successfully evaded immune rejection from the recipient mice.
While the previous technique developed by Dr. Shi’s team involved creating a personalized cell therapy using the patient’s own cells to prevent immune rejection, this new approach utilizes techniques that enable hypoimmunogenic cells engineered from healthy donors to be transplanted into a disease model without triggering an immune response that would harm the therapeutic cells.